Takeaway
A bolus of 1.5 mg/kg, followed by an infusion of 2 mg/kg/h until the end of the surgery can help reduce postoperative laryngopharyngeal symptoms, including sore throat, hoarseness, and cough, without increasing adverse reactions.
Design
- Prospective, randomized, double-blind, controlled, single-center clinical trial with 160 patients.
- Inclusion criteria: men or women aged 20–60 years old, American Society of Anesthesiologist (ASA) class I or II, Mallampati class I or II, body mass index < 30 kg/m2, no sore throat prior to the procedure
- Exclusion criteria: conversion to ETT, LMA insert attempts ≥ 2), history of laryngitis and GERD, upper respiratory tract infection in the past 2 weeks, actively smoking, obvious abnormalities in liver or kidney function, allergy to local anesthetics (including but not limited to lidocaine) and operative time > 120 min
- Randomly divided into control group (Group C), lidocaine gel group (Group LG), intravenous lidocaine group (Group SL) and continuous infusion of lidocaine group (Group CL) on a 1:1:1:1 basis
- Primary outcomes were the incidence and severity of POST at the time of LMA removal (T1), 2 h (T2), 6 h (T3), and 24 h(T4) after removal
Physiology Refresh
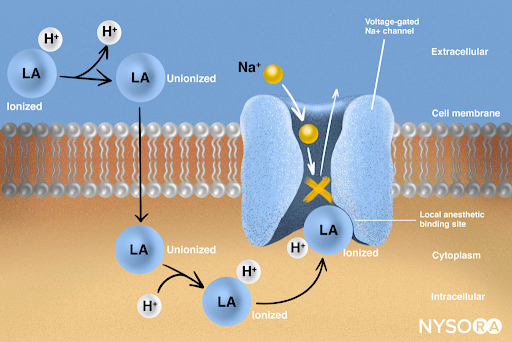
Nerves fire by depolarizing—sodium (Na⁺) rushes in, triggering an action potential that travels the length of a nerve.
Local anesthetic molecules exist in ionized and unionized states. The unionized state allows molecules to cross the cell membrane, but they rapidly ionize and plug voltage-gated Na⁺ channels. Channel blockade occurs in a reversible and concentration dependent manner - preventing Na⁺ entry and slowing depolarization
→ No action potential → No nerve signal.
Threshold is not reached, preventing the wave of pain signal transmission down the length of the nerve.
Excerpts
Within 24 h after extubation, the incidence of POST was significantly lower in group CL than in group C at all time points
number of patients with mild pain in group CL was less than that in group C at all time points, and there was no moderate or greater pain in group CL
incidence of hoarseness and cough in group CL were significantly lower than that in group C
lidocaine reduced the incidence of POST, with a bolus of 1.5 mg/kg, followed by an infusion of 2 mg/kg/h being the most effective. Furthermore, continuous infusion of lidocaine decreased the incidence of other postoperative laryngopharyngeal symptoms, including hoarseness and cough. And lidocaine did not increase the risk of other adverse reactions.
The etiology of POST is multifactorial, including age, insertion method and techniques, size and cuff pressure of laryngeal mask, trauma during airway insertion and suctioning, and type of surgery
Lidocaine, one of the most widely studied drugs for the treatment of POST, suppresses the airway’ s excitatory sensory C fibres and the release of sensory neuropeptides, which in turn reduces laryngeal irritation and inflammation
we found that a single bolus of lidocaine reduced the incidence of POST only at the time of laryngeal mask removal. In contrast, a continuous infusion of lidocaine reduced the incidence of POST within 24 h after extubation. And there was no more than moderate pain at any time since the operation. This may be due to the fact that the half-life of i.v. lidocaine is approximately 1.5 h. In our study, the duration of surgeries were less than 2 h, suggesting that a single bolus of lidocaine may indeed reduce the incidence of POST by virtue of lidocaine reaching clinically significant plasma concentrations at the time of extubation, but this effect cannot be extrapolated to longer postoperative periods or to surgeries of longer duration.
Abstract
Background
This randomized controlled trial was performed to explore efficacy of continuous intravenous infusion of lidocaine on postoperative sore throat after laryngeal mask insertion.
Methods
In this prospective trial one hundred and sixty general anesthesia surgery patients (20 to 60 years) using laryngeal mask airway were randomly divided into control group (Group C, saline as placebo), lidocaine gel group (Group LG, lidocaine gel applied to the surface of the laryngeal mask), single intravenous lidocaine group (Group SL, intravenous lidocaine 1.5 mg/kg at induction of anesthesia) and continuous infusion of lidocaine group (Group CL, a bolus of 1.5 mg/kg, followed by an infusion of 2 mg/kg/h until the end of the surgical). The primary outcomes were the incidence and severity of POST at the time of laryngeal mask removal (T1), 2 h (T2), 6 h (T3), and 24 h (T4) after removal. The secondary outcomes included the incidence of adverse events such as hoarseness, cough, and tongue numbness.
Result
Within 24 h after extubation, the incidence and severity of POST was significantly lower in group CL than that in group C at all time points. In contrast, compared with group C, the incidence and severity of POST in group SL was lower only at T1. The incidence of hoarseness and cough in group CL were significantly lower than that in group C at T1 and T2. In group SL, the incidence of hoarseness and cough was lower than that in the group C only at T1. In group LG, the incidence of tongue numbness was significantly higher than that in group C only at T1, and there were no significant difference in the four groups at the other time points.
Conclusion
Continuous infusion of lidocaine is effective in reducing the incidence and severity of POST after laryngeal mask ventilation, as well as reducing the incidence of adverse effects such as hoarseness and cough.
Citation
Jiang J, Wu J, Shi S, Dong X, Yin J, Wu Y. Efficacy of continuous intravenous infusion of lidocaine on postoperative sore throat after laryngeal mask insertion: a randomized controlled trial. BMC Anesthesiol. 2025 Feb 8;25(1):63. doi: 10.1186/s12871-025-02937-y. PMID: 39923028; PMCID: PMC11806593.
