Understanding Pulse Oximeter Plethysmography (POP)
Pulse oximeter plethysmography (POP) provides more than just oxygen saturation data. By interpreting its waveform, anesthesia providers can learn about a patient’s cardiovascular status and fluid responsiveness.
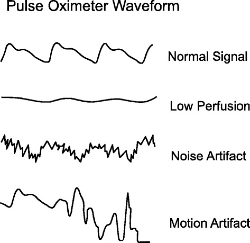
Waveform Morphology
The POP waveform is created from infrared light signals, which are less affected by changes in oxygen levels.
Normal Waveform: Looks like asymmetric humps, similar to an arterial pressure waveform but less detailed.
Vasomotor Tone
Waveform changes reflect blood volume and vascular resistance:
- Amplitude:
- Higher amplitude = vasodilation (more light reaches the detector).
- Lower amplitude = vasoconstriction (less light reaches the detector).
- Dicrotic Notch:
- In vasoconstriction, the notch is above 50% of waveform height.
- In vasodilation, the notch is below 50%.
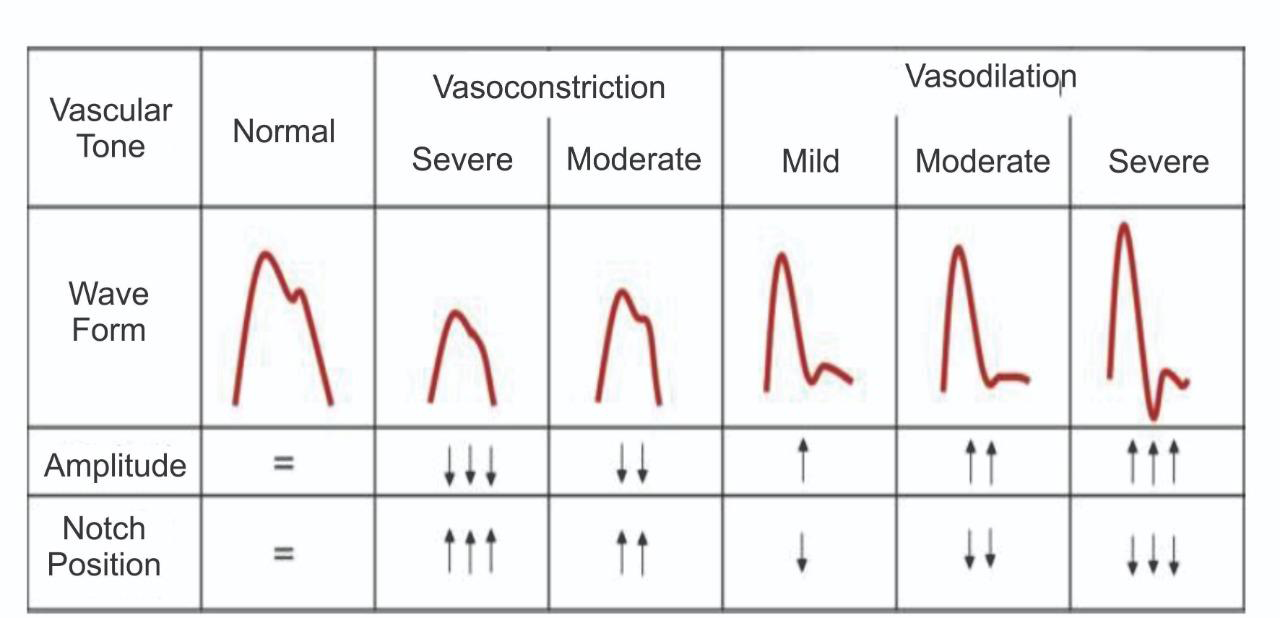
Notice the amplitude and notch position are in opposition to one another.
Clinical Tip
Local vasodilation can indicate a successful nerve block due to anesthesia-induced sympathectomy.
Perfusion Index (PI)
PI quantifies vasomotor tone as: (AC/DC) × 100%.
- Low PI: Suggests vasoconstriction or severe hypovolemia.
- High PI: Indicates vasodilation.
PI is influenced by finger temperature, vasoactive drugs, sympathetic tone (e.g., pain/anxiety), and stroke volume.
Respiratory Variations
POP waveforms change with intrathoracic pressure during breathing.
- Positive Pressure Ventilation:
- Inhalation increases intrathoracic pressure, decreasing venous return and stroke volume.
- Exhalation reverses this effect.
These changes can predict fluid responsiveness:
- Significant amplitude variations (>13% ∆POP) suggest responsiveness.
The same mechanism is responsible for pulse pressure variation (PPV) when monitoring an arterial line. The dampening effect is reflected in an altered pulse oximetry light absorption.
Interpreting respiratory variations:
- Significant variations in waveform amplitude (∆POP) during mechanical ventilation may indicate fluid responsiveness. Although studies focus on positive pressure ventilation, it can also be measured and trended during spontaneous respiration.
- A threshold ∆POP > 13% has been shown to predict fluid responsiveness with high sensitivity and specificity.
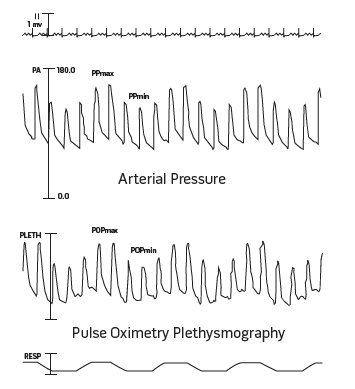
These respiratory variations become more pronounced in a hypovolemic patient. However, they can be difficult to detect with the naked eye, unless profound hypovolemia exists. This is where the PVI comes in.
Pleth Variability Index (PVI)
PVI measures changes in PI during respiratory cycles:
PVI = (PI max - PI min)/PI max × 100%.
- High PVI (>14%): Predicts fluid responsiveness in ventilated patients.
PVI is a metric available on Philips monitors, but the institution must purchase the rights to display the algorithm.
The respiratory variations can be difficult to visualize in an anesthesia monitor's normal settings. Fortunately, there's a workaround to better visualize the undulations.
Clinical Pearl
Select the pulse ox waveform and change the "Speed" to 6.5 mm/sec. This condenses the waveform and makes the respiratory cycles easier to visualize.
Make this change is prior to induction of general anesthesia - respiratory variations can predict post induction hypotension.
Cardiopulmonary Resuscitation (CPR) Quality
Emerging research suggests that POP waveform analysis during CPR may provide valuable information.
Interpreting during CPR:
- POP amplitude and area under the curve correlates with higher-quality CPR, coronary perfusion pressure, and end-tidal CO2 in animal studies.
- POP may help in identifying return of spontaneous circulation (ROSC) during active CPR.
Airway Obstruction Assessment
Changes in the POP waveform can reflect the severity of airway obstruction.
- Increased variability in waveform amplitude may indicate worsening obstruction.
Conclusion
Pulse oximeter plethysmography offers anesthesia providers a non-invasive tool to assess various aspects of patient physiology. By carefully interpreting the waveform characteristics, clinicians can gain insights into perfusion, fluid status, airway obstruction, and even CPR quality. As with any clinical tool, POP should be used in conjunction with other assessments and the overall clinical picture to guide patient management decisions.
Citations
- Arnold DH, Spiro DM, Desmond RA, Hagood JS. Estimation of airway obstruction using oximeter plethysmograph waveform data. Respir Res. 2005 Jun 28;6(1):65. doi: 10.1186/1465-9921-6-65. PMID: 15985171; PMCID: PMC1168908.
- Pérez Nieto, Orlando & Guerrero Gutierrez, Manuel & Soriano, Raul & Deloya Tomas, Ernesto & López, Eder Iván & Lopez Fermin, Jorge. (2020). Hemodynamic Monitoring with the Clinic: Back to Basics.
- Cannesson M, Talke P. Recent advances in pulse oximetry. F1000 Med Rep. 2009 Aug 26;1:66. doi: 10.3410/M1-66. PMID: 20948714; PMCID: PMC2948314.
- Kim YJ, Seo JH, Lee HC, Kim HS. Pleth variability index during preoxygenation could predict anesthesia-induced hypotension: A prospective, observational study. J Clin Anesth. 2023 Nov;90:111236. doi: 10.1016/j.jclinane.2023.111236. Epub 2023 Aug 26. PMID: 37639751.
- Masimo Corporation. (2008). Plethysmographic waveform: Technical bulletin. Masimo Corporation.
- Xu J, Li C, Tang H, Tan D, Fu Y, Zong L, Jing D, et al. Pulse oximetry waveform: A non-invasive physiological predictor for the return of spontaneous circulation in cardiac arrest patients -— A multicenter, prospective observational study. Resuscitation. 2021 Dec;169:189-197. doi: 10.1016/j.resuscitation.2021.09.032. Epub 2021 Oct 6. PMID: 34624410.
Additional References
- Pleth variability index: A dynamic measurement to help assess physiology and fluid responsiveness. (n.d.). Retrieved from https://anesthesiology.queensu.ca/sites/anesthesiology/files/inline-files/LAB4583B_Technical_Bulletin_Pleth_Variability_Index.pdf
- Feissel, M., Teboul, J. L., Merlani, P., Badie, J., Faller, J. P., & Bendjelid, K. (2007). Plethysmographic dynamic indices predict fluid responsiveness in septic ventilated patients. Intensive Care Medicine, 33(6), 993-999. https://pubs.asahq.org/anesthesiology/article/106/6/1105/8177/Respiratory-Variations-in-Pulse-Oximetry
- Garde, A., Zhou, G., Raihana, S., Dunsmuir, D., Karlen, W., Dekhordi, P., Huda, T., Arifeen, S. E., Larson, C., Kissoon, N., Dumont, G. A., & Ansermino, J. M. (2020). Measuring accuracy of plethysmography based respiratory rate measurement using pulse oximeter at a tertiary hospital in India. Pneumonia, 12(1), 4. https://pneumonia.biomedcentral.com/articles/10.1186/s41479-020-00067-2
- Jubran A. Pulse oximetry. Crit Care. 2015 Jul 16;19(1):272. doi: 10.1186/s13054-015-0984-8. PMID: 26179876; PMCID: PMC4504215.
- Reisner, A., Shaltis, P. A., McCombie, D., & Asada, H. H. (2008). Utility of the photoplethysmogram in circulatory monitoring. Anesthesiology, 108(5), 950-958. https://pmc.ncbi.nlm.nih.gov/articles/PMC8762650/
- Shepard LN, Berg RA, Morgan RW. Pulse oximetry plethysmography: A new approach for physiology-directed CPR? Resuscitation. 2021 Dec;169:198-200. doi: 10.1016/j.resuscitation.2021.10.039. Epub 2021 Oct 29. PMID: 34757060; PMCID: PMC8762650.
Pulse Oximeter Plethysmography: A Window into Patient Physiology
Pulse oximeter plethysmography (POP) provides more than just oxygen saturation data. By interpreting its waveform, anesthesia providers can learn about a patient’s cardiovascular status and fluid responsiveness.
